The Medicine Of The Future
Health System Reform Program With Focus On Prevention And Causal Therapy: A Comprehensive Approach To Reforming The Physical, Mental And Social Health & Wellbeing Of Society
Introduction
The history of medicine traces a significant evolution. The medical understanding that fundamental human needs—such as nutrition, sleep, physical activity, and social connection—are essential to health traces back to the teachings of Hippocrates of Kos. He emphasized the importance of living in harmony with nature. On this basis, two and a half thousand years ago, he developed a primarily preventive, systemic and deeply natural approach to medicine. Together with his students, he laid the foundations for nature-oriented medicine as an empirical science: health or illness were not random or fated developments, but had natural causes that – once understood - could also be influenced in natural ways. Man was thus not the plaything of divine whim but, like all life, part of nature and subject to its laws. With this revolutionary view, he undermined the almost absolute power of the priestly word in matters of illness and freed medicine from faith: it is not gods on Mount Olympus or elsewhere that cause illness and suffering, but a way of life that is not in harmony with natural needs. But the early 20th century saw the influence of Rockefeller medicine, which promoted exclusively a pharmaceutical-oriented approach. This led to the gradual exclusion and prohibition of natural medical practices such as osteopathy or herbal medicine, presenting them as less credible "alternative" medicine, as if the laws of nature did not apply to humans (see below, the Law of Minimum and Maximum required for healthy homeostasis). But there is no humane alternative to medical practice that respects natural human needs.
As medicine has become increasingly institutionalized, its focus has shifted toward symptom-oriented approaches—often at the expense of holistic care and an understanding of patients within the broader context of their life stories. Modern medicine largely emphasizes biomedical models that prioritize isolated physical symptoms.
Yet there is a growing awareness of the need for a more comprehensive approach—one that seeks to harmonize the individual with their environment on physical, emotional, mental, and spiritual levels.
The current system is rooted in the economics of medicine and has evolved into a disease management industry—not designed to cure, but to keep people on lifelong medications. It's no longer a healing art grounded in a deep understanding of human needs, but a business model. The growing number of children being chronically medicated highlights the serious consequences of this unhealthy cultural trend—and underscores the urgent need to shift toward a more integrated, holistic approach to health in the future of modern healthcare. Reforming the system requires a renewed ethos—one grounded in shared ethics and a commitment to personal responsibility.
Christof Plothe (DO), who contributed to this document by preparing it for international publication and suggesting additions, is the Health & Science Committee Lead at The World Council for Health. The Council proposes the five sound Better Way Principles as the foundational ethos for the health systems reform outlined in this document. The Better Way Principles are:
We act in honour and do no harm.
We are free beings with free will.
We are part of nature.
Spirituality is integral to our well-being.
We thrive together.
We value different perspectives.
We use technology with discernment.
Underlying these principles is the assurance that we do not tolerate the violation of inalienable rights and freedoms, and we do not tolerate profit, power and influence coming before the wellbeing of people and the earth.
Table of contents
1. GENERAL PRINCIPLES
1.1 Priority of a Species-Appropriate, Disease-Preventing and Causal-Therapeutic Lifestyle
1.2 Systemic Approach Instead of Reductionism
1.3 The Laws of the Minimum and the Maximum as the Foundations of Preventive Medicine
1.4 Respect for Personal Autonomy
1.5 Combating Corporate Corruption
1.6 Disease Prevention and Protection Against Pharmaceutical Intoxication
2. CONCRETE PREVENTIVE MEASURES AND STRATEGIES
2.1 Promoting and Strengthening Personal Responsibility
2.2 Reforming the Influence of Industry on Politics, Research, Teaching and Public Life
2.3 Reforming the Health Insurance and Medical Reimbursement System
2.4 Reforming Medical and General Curative Education Courses and Curricula
2.5 Legal Measures to Protect the Population
3. FINAL REMARKS
1. GENERAL PRINCIPLES
1.1. Priority of a species-appropriate, disease-preventing and causal-therapeutic lifestyle
Modern medicine has made tremendous strides, especially in acute care through medication and in surgical trauma treatment. However, when it comes to the rising epidemic of so-called lifestyle diseases, the solutions are often ineffective. This stems from a fundamental flaw in the global system: Multicausal problems can't be solved with single-cause solutions, and symptom-based interventions often make things worse by masking the root issues while serving market interests.
The Need for a Personalized and Holistic Approach
There’s an urgent need to return to a model where medical decisions are guided by doctors and healthcare practitioners based on individual patient needs—not dictated by industry-sponsored guidelines. This shift would empower practitioners to consider the unique circumstances of each individual, promoting a more personalized and holistic approach to health. Pregnancy, birth, and perinatal care are also critical areas of health that demand greater attention. This period is foundational for both maternal and child health, influencing long-term outcomes. Emphasizing comprehensive care during this time can foster healthier generations.
Additionally, incorporating health education into child education is essential for fostering a health-conscious society. By teaching children about health from an early age, we can encourage personal responsibility and informed decision-making regarding their well-being.
The only viable solution to the challenges posed by lifestyle diseases is a multi-causal approach. This involves a return to a species-appropriate lifestyle under modern conditions, promoting a health-conscious society that encourages personal responsibility. By integrating a focus on perinatal health, empowering healthcare practitioners, and emphasizing health education, we can create a more holistic and effective healthcare system.
1.2 Systemic Approach Instead of Reductionism
Multicausal health problems—responsible for over 90% of all chronic illnesses, including so-called diseases of civilization (such as depression, anxiety disorders, Alzheimer's, metabolic and cardiovascular diseases, and many major forms of cancer), as well as numerous developmental and neuropsychiatric disorders (including autism, schizophrenia, and bipolar disorder)—represent both the greatest challenge and the greatest opportunity for preventive and causally-oriented therapeutic solutions. This is true for two main reasons:
They are incurable with medication alone, because no drug can substitute for the essential elements whose absence lies at the root of these chronic conditions.
Only a systems-based medical approach—rooted in a deep understanding of human nature—can deliver truly effective prevention and address the root causes of disease.
Preventing and treating multicausal diseases requires a systems-based approach that gives equal weight to environmental factors (such as toxins), deficiencies in essential nutrients, and lifestyle choices. Today’s “normal” is often mistaken for “natural,” and mere correlations are frequently misinterpreted as causation—often with devastating consequences for public health. For example, age is commonly cited as the primary risk factor for Alzheimer’s disease, even though this correlation merely reflects the time it takes for the consequences of an unhealthy lifestyle to manifest clinically. There are many ways to destroy mental health, so there is no single drug that will ever change the course of the disease. Prevention requires that these pathways be recognized, understood, and offered to the public (e.g., Nehls M: Unified theory of Alzheimer’s disease (UTAD): implications for prevention and curative therapy).
Pinpointing individual decisive factors can be meaningful in specific cases and may offer practical value, but in scientific research, effective prevention and treatment require multicausal approaches rooted in systems thinking. Due to the multi-causal character of diseases, classic mono-causal intervention studies based on pharmaceutical principles must fail and are therefore not an option.
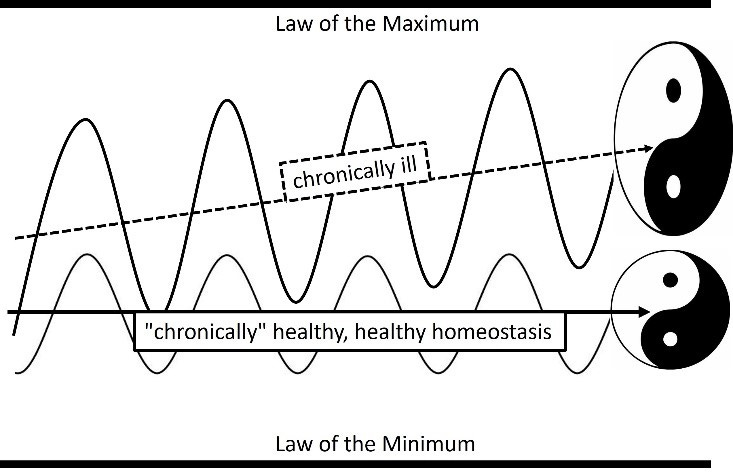
The goal is to strengthen the body's natural ability to maintain healthy homeostasis. This approach minimizes the risk of acute, life-threatening events—such as infections—that pose little danger when the physical immune system is intact, as well as chronic conditions like post-traumatic stress disorder, which can develop from stressful experiences that might have been overcome had the mental immune system not been impaired in its natural function. To successfully navigate such natural challenges—and even strengthen long-term health—the principles of minimum and maximum must be observed. These principles highlight the need for personalized solutions aimed at restoring and maintaining homeostasis.
1.3 The laws of minimum and maximum, homeostasis and synergetic effects as the foundation of preventive medicine
The Law of the Minimum is a fundamental principle that underscores the critical role of essential factors in human health and development. It holds that a significant deficiency in any one vital element can impede growth, function, and well-being—regardless of the adequacy of other factors. For example, a deficiency in vitamin D3 cannot be compensated by increasing iodine or selenium intake. Each vital nutrient—or any other essential factor—is unique and irreplaceable. This, by extension, also applies to pharmaceutical drugs. Therefore, relying on drugs to address health problems caused by an inappropriate lifestyle with key deficiencies must, by simple logic, be ineffective.
The Law of the Maximum describes the principle that excessive harmful influences—such as chronic stress or environmental toxins—can overwhelm the body’s ability to maintain homeostasis, ultimately leading to serious health issues. This overload can trigger acute, life-threatening conditions or contribute to the gradual development of chronic diseases that are increasingly common in modern societies. Logically, the combined effect of two or more substances is greater than the sum of their individual effects. This is especially true when the body is already struggling to maintain homeostasis due to a violation of the Law of the Minimum—even in the absence of toxins. In such cases, the system becomes less able to tolerate additional toxic stressors, and conversely, the presence of these stressors further exacerbates existing deficiencies.
The word Homeostasis, life’s dynamic equilibrium between the laws of minimum and maximum, is derived from the ancient Greek words homoios, meaning "equal," and stásis, meaning "standstill". However, this state is only apparently still, as there is nothing static in nature, but rather always a dynamic balance of forces, which is why "equilibrium" is the better translation and has caught on. Like riding a bicycle, stability can only be achieved through movement. The Greek philosopher Heraclitus (520-460 B.C.) is credited with the insight panta rhei, ancient Greek for "everything flows," which is also true of our current physical understanding of the universe and everything within. Life, by its very nature, depends on constant interaction with its environment. In other words: there can be no life without dynamic exchange—and no life without balance. We therefore live in a constant state of tension between the Law of the Minimum and the Law of the Maximum, as illustrated in the figure above. It becomes clear how an unhealthy lifestyle—over time and with inevitability—leads to a chronic state of disease.
Furthermore, unless the Law of the Minimum is acknowledged—which, notably, is not currently part of medical education in Germany—medications can only provide symptomatic relief. Without addressing the root causes of disease, such treatment rarely leads to true healing. In fact, except in rare cases where a drug replaces an actual deficiency (such as insulin in type 1 diabetes), purely symptomatic therapy may paradoxically sustain chronic illness by masking symptoms and thereby reinforcing an unhealthy status quo. Thus, while symptomatic treatments may appear to bypass the Laws of the Minimum and Maximum in both life and medicine, they often eliminate the motivation to address the root causes of illness through meaningful lifestyle changes—since taking a prescription becomes the simpler and more convenient option.
1.4 Respect for Personal Autonomy: A Pro-Human Health Policy Centered on Human Dignity and Sovereignty
Respect for human dignity and sovereignty is integral to pro-human health systems that focus on the natural needs of human beings. This respect encompasses the unrestricted right to lead a self-determined life, which includes the possibility of choosing an unhealthy diet or lifestyle of one's own free will. However, it is essential to ensure that every person is informed about the decisive factors affecting their health and has the concrete opportunity to align their lives accordingly, whenever and to whatever extent they make this decision.
Central to this approach is the principle of informed consent, which empowers individuals to make knowledgeable choices regarding their health and treatment options. This means individuals must be fully informed about the potential benefits and risks of any medical intervention, enabling them to actively participate in decisions about their own health. Accordingly, no medical treatment or vaccination should ever be mandatory in a way that overrides personal autonomy. People must retain the freedom to accept or decline medical interventions based on their own values and beliefs.
Moreover, medicine should be understood as a cooperative endeavor between the individual seeking health and the one offering support—more accurately described as a health supporter, since true health can only be provided by nature. This partnership fosters open communication, mutual respect, and shared decision-making, ensuring that healthcare is tailored to each person's unique needs and values. Such collaboration not only strengthens the therapeutic relationship but also leads to improved health outcomes.
1.5 Combating Corporate Corruption
A major reason for the widespread failure in preventing and treating lifestyle-related diseases—including the purported prevention of infectious diseases through mass vaccination campaigns—is a fundamental flaw in health policy: the undue influence of profit-driven corporations on public health authorities and regulatory institutions. This influence often results in scientific evidence being ignored, misrepresented, or manipulated to serve economic interests. Over the past decades, the pharmaceutical industry has increasingly brought health agencies, regulatory bodies, and political decision-makers under its control. One striking example is the case of the genetically modified COVID-19 "vaccine," where safety studies were not conducted independently, and regulatory agencies not only failed to uphold oversight but actively served industry interests—at the expense of public well-being. To protect public health, it is imperative that corporate influence over governmental and regulatory institutions be ended without delay.
1.6 Prevention of Disease and Protection Against Pharmaceutical Intoxication
Our culture has been deeply shaped by the interests of the pharmaceutical industry, which employs multilayered propaganda to implant a fundamental—and false—assumption about human nature: that humans are inherently flawed. From this perspective, illness is inevitable. This misconception is insidiously reinforced by portraying a species-appropriate, health-promoting lifestyle as unrealistic or even absurd. As a result, personal responsibility is often dismissed—after all, “why change your lifestyle if it doesn’t matter?” This highlights the urgent need for widespread education as the foundation for a new health culture.
At the heart of this misdirection lies a dogma promoted by the pharmaceutical industry and instilled in medical students from the very beginning of their training. It is built on five axioms—unproven, often unprovable assumptions—accepted without question and rarely, if ever, challenged.
Illness is seen as a natural, inevitable process—one that simply becomes symptomatic with advancing age.
The tendency to develop certain diseases is often attributed to inherited genes—suggesting that the human body is inherently flawed by design.
Consequently, lifestyle is regarded as having little to no impact on health. Supplying the body with essential nutrients—even when they are clearly lacking in the diet—is dismissed as unnecessary, a waste of money, or even a potential health risk.
The question of which disease will ultimately develop—be it cancer, Alzheimer’s, diabetes, or another—is left to chance, as if drawn from the roulette wheel of life.
As a logical consequence of these beliefs, only pharmaceutical research—and its arsenal of synthetic drugs—is seen as capable of protecting humanity from suffering and premature death.
In transhumanist thinking, the ultimate goal is nothing less than the abolition of death itself—achieved through technological means. Yet advocates of such views would do well to reflect on the fact that even the noblest of intentions often lead to the very oppo
site of what they seek to achieve.
While the number of preventable diseases continues to rise sharply, an estimated 882,000 people die each year in the United States alone as a result of prescription drugs—making them the leading cause of death. Among these, psychotropic medications rank as the third most common cause, alongside painkillers. This alarming figure highlights the urgent need to shift focus toward natural and nature-based treatment approaches, to restrict prescriptions to truly essential cases, to establish independent oversight mechanisms, and to expand public education on healthy lifestyles and effective non-pharmaceutical alternatives.
In short: we must reestablish a culture of trust in the body’s innate capacity to heal—a process that should be supported, not overridden.
In addition, all scientific studies and approval processes must be subjected to review by independent scientists with no ties to industry. For products already on the market, retrospective, industry-independent evaluations must be conducted. Going forward, only health measures that are truly necessary and evidence-based should be recommended and publicly funded—everything else must be phased out. The financial resources thus freed must be reinvested in disease prevention and causal, system-based therapies.
To minimize the risk posed by harmful medications, manufacturers must be held fully accountable for the safety and consequences of their products.
2. CONCRETE PREVENTIVE MEASURES AND STRATEGIES
2.1 Promoting and Strengthening Personal Responsibility
A return to species-appropriate living conditions—adapted to modern realities—is essential for preventing the multicausal diseases of civilization that place an unnecessary burden on individuals, families, and society as a whole. Since these diseases stem from a lifestyle misaligned with human nature, addressing them requires a fundamental restructuring of the current healthcare system, which—under the influence of industrial interests—often promotes illness rather than health.
The ongoing trend toward over-medicalization illustrates how diseases are increasingly managed through one-sided pharmaceutical strategies, rather than through holistic, cause-oriented approaches. This underscores the urgent need to strengthen systemic thinking and to prioritize natural and integrative alternatives.
Healthy behavior and recovery cannot be outsourced—they are the personal responsibility of each individual. However, the goal of any effective program must be to introduce people to this self-concept and empower them to take ownership of their health—without condescension or paternalism:
Promote a self-image of the human being that recognizes the innate ability to heal and maintain health—provided that species-appropriate conditions are in place.
Foster media literacy to empower individuals to distinguish facts from opinions and to recognize manipulative narratives.
Launch educational campaigns to raise awareness of the importance of balanced nutrient intake and to provide practical, voluntary strategies for achieving it—potentially including the subsidization of essential nutrients, such as algae oil.
Strengthen mental resilience through programs that focus on stress management, emotional intelligence, and critical self-reflection as core components.
Foster individual responsibility by improving access to reliable health information and services, empowering people to make informed decisions. Include training in stress management and conflict resolution.
Include preventive measures that encompass both social and emotional health.
Strengthen community structures through initiatives that promote social connection, cooperation, and supportive networks.
Empower individuals through education on health, justice, and sovereignty—promoting meaningful change by offering real hope for a better future, rooted in a society of individuals with a well-functioning mental immune system, which is essential for any true democracy.
2.2 Living Solidarity
Although many lifestyle-related diseases can be prevented through effective measures, a fair and accessible healthcare system remains indispensable—not only as a safety net for those already affected, but also as a foundation for a healthy and productive society. Such a system guarantees dignified access to care for all individuals, regardless of their personal choices.
In the long term, this approach will reduce healthcare costs, as a more health-conscious population leads to fewer chronic illnesses, and treatment strategies are guided by actual effectiveness rather than short-term profit motives. A health-oriented and preventive model acknowledges the importance of:
Reignite awareness of a more natural, balanced way of living through targeted initiatives in schools and workplaces.
Natural Nutrition
Subsidies for organic food and sustainable agriculture, alongside a step-by-step but rapid phase-out of pesticides and other environmentally harmful substances.
Harmful additives such as aluminum, trans fats and glucose-fructose The elimination of harmful additives like aluminum, trans fats, and glucose-fructose syrup in favor of healthier alternatives. Public subsidies for sugar and ultra-processed foods must be discontinued.
Drastically reducing the use of antibiotics in livestock farming to curb the rise of resistant bacteria, which represent a serious and escalating danger to public health.
A complete stop to the use of genetic vaccines in livestock, as a precautionary measure to avoid the introduction of inadequately tested biotechnologies into the food chain.
Ensuring that consumers are fully informed about what is in their food and how it is produced—only then can they make responsible choices for their health. Misleading advertising must become a thing of the past.
Comprehensive, voluntary diagnostic services for nutrient deficiencies—financed by health insurance providers that truly promote health rather than pharmaceutical profits—using standardized blood tests for key micronutrients such as 25-hydroxyvitamin D3, marine omega-3 fatty acids, vitamin B12, and essential trace elements like magnesium, iodine, and lithium.
2.2 Reform of the Pharmaceutical Industry's Influence on Politics, Research, Teaching and Public Life
The goal of health system reform must be to ensure political transparency and independence from the interests of the pharmaceutical industry. After all, the mandate of elected representatives—to serve the health and well-being of the people—is fundamentally at odds with the profit-driven objectives of pharmaceutical corporations and the institutions tied to them. While policymakers are meant to act in the public interest, the pharmaceutical industry is accountable primarily to its shareholders and profits most from a chronically ill population. Without effective political regulation, genuine health policy reform remains out of reach.
Improving Healthcare Guidelines
So-called scientific medical associations are not suited to develop guidelines that truly reflect current scientific knowledge and prioritize human well-being. Instead, such guidelines must be formulated by genuinely independent experts. Many association members maintain close ties to the pharmaceutical industry, which often rewards physicians who promote its products—with speaking engagements, career-advancing awards, and influential positions. These same individuals may also contribute to the development of official guidelines, while their connections to industry-sponsored associations undermine both their objectivity and the credibility of the recommendations.
Proof of Efficacy and Safety
Historically, drug approvals have required proof of only a single effect—yet this does not guarantee real-world health benefits. For example, cholesterol-lowering medications may effectively reduce cholesterol levels, but this does not necessarily translate into improved overall health or increased longevity in otherwise healthy individuals. For this reason, clinical studies must go beyond isolated effects: they must demonstrate clear, meaningful benefits and include long-term follow-up of those receiving the treatment.
However, clinical trials conducted by pharmaceutical manufacturers often present overly optimistic results—reporting higher efficacy and fewer side effects compared to independent studies. This distortion is driven by a range of factors, including selective publication of favorable outcomes, study directors who shape results to secure future contracts, and direct pressure from clients on research teams. Such practices compromise the integrity of the scientific evidence base that informs global pharmaceutical policy.
Preventing Industry Influence
Corporate influence over politicians and regulators must be fully exposed—and lobbying by corporations must be recognized for what it is: a conflict with democratic principles. Any attempt to merge corporate interests with the responsibilities of public representatives must be considered a serious violation and be subject to criminal prosecution.
All third-party influence over national healthcare policy must end—without exception. This includes withdrawing from international agreements and organizations, such as the WHO and its International Health Regulations, where they compromise national health sovereignty. No institution, corporation, or unelected body should have the authority to dictate how a sovereign population manages its health.
To ensure this, concrete measures must be implemented:
Establish robust accountability structures
Create an independent oversight body to uncover and restrict the influence of corporate funding in politics.
Introduce mandatory cooling-off periods—or even full bans—on transitions between public offices and related private sector positions to prevent the revolving door effect.
Strengthen integrity through binding transparency rules, requiring the disclosure of all professional affiliations, monitored by an independent authority.
Prohibit commercial advertising of medical products
Beyond independent information, no public advertising of medical products shall be permitted. Health decisions must be based on education, not marketing.
Mandate full disclosure of conflicts of interest in scientific and public health communication
Complete transparency must be ensured in all scientific publications, guideline development, and public appearances. All financial ties and political or industrial influences must be declared.
Non-disclosure must be treated as a criminal offense—because where human health is at stake, concealment is not a minor oversight, but a serious crime.
Mandatory Study Registers for Industry and Military Studies
Implementing mandatory study registers for industry and military studies is essential. A significant advancement in this area would involve establishing mandatory, publicly accessible registers for clinical studies across Europe. Every medical study would need to be registered prior to its commencement, with detailed explanations of the study design and endpoints. Furthermore, each study should be published promptly after its completion. This approach would effectively combat selective publication and the retrospective alteration of endpoints or study designs, representing a major leap forward towards creating a transparent database for accurately assessing the effectiveness of pharmaceuticals. It would also prevent the conduct of bioweapons and gain of function research.
2.3 Reform to Payments of Health Care Practitioners, Health Insurance and Medical Reimbursement System
Dignified working conditions for people within the healthcare system are vital. Healthcare practitioners must be supported in their roles, as their well-being directly impacts the quality of care they provide. Since medicine today is predominantly driven by economic incentives, some countries have transitioned to paying medical experts on a flat-rate basis. This approach ensures stable income without incentivizing unnecessary interventions. A similar model existed in hospitals until the 1990s, after which privatization forced institutions to prioritize financial survival over patient care. To ensure health insurance funds become true health funds, reform of the payment system includes:
Higher reimbursement for preventive measures in the health care system
Health seeker education in medical practices in the direction of educating on causal disease prevention and therapy options should be made more lucrative by increasing fees
Models should be developed in which doctors are rewarded for maintaining the health of the populations they serve.
Promotion of educational campaigns that encourage a species-appropriate, health-promoting lifestyle.
2.4 Reform of Medical and General Health Professional Courses and Curricula
Integrate a holistic vision of the human being—as physical, emotional, mental, and spiritual—into all educational curricula, emphasizing systemic and causal approaches to disease prevention and therapy. This includes teaching the Laws of Minimum and Maximum as foundational principles, alongside systems biology as the scientific basis for maintaining homeostasis, optimal child development, and long-term health.
Integration of toxicology (chemical, metal, electromagnetic fields (EMF), etc.) by teaching the connection of a healthy human and a healthy environment.
Redefine health and health promotion as the preservation and restoration of balance, rather than the mere suppression of symptoms. This requires banning pharmaceutical industry-sponsored medical education and ensuring that universities are funded independently through public resources.
2.5 Legal Measures for the Protection of the Population
Reduction of harmful environmental influences:
Legal measures should re-evaluate and redefine limits for exposure to environmental toxins, microplastics, aluminum, drug residues, particulate matter and toxic food components without the influence of the respective industries.
The same applies to EMF (including 4G and 5G): while the use of modern technologies like mobile phones should remain possible, wireless networks that may be harmful to brain development must be phased out—especially in sensitive environments such as schools and kindergartens. In these settings, innovative alternatives with no known adverse health effects—such as LiFi technologies—should be implemented wherever feasible. This ensures that modern functionality and health protection are not mutually exclusive, but mutually reinforcing.
In addition, funding programs should be set up to cover the costs of individual shielding measures, thus facilitating protection in private and professional spaces.
Ensuring the safety and efficacy of medical products:
Every manufacturer must be fully liable for the safety of its products.
Pharmaceutical products may only be approved or continue to be marketed if their safety has been unequivocally demonstrated by independent, controlled studies.
Vaccines—because they are administered to healthy individuals who may never fall ill—must be subject to the strictest approval standards. They should only be authorized or continue to be marketed if their safety and efficacy have been unequivocally demonstrated through independent, controlled studies that include comparisons with the best available natural alternatives (e.g., vitamin D supplementation versus a vaccine for respiratory infections).
All drugs that come onto the market must be reviewed by independent experts; ideally, studies should be state-funded as long as the guidelines and allocation of funds are determined by independent expert committees that are not tied to industry or party politics.
Independent replication of landmark studies with significant public health implications—such as those evaluating the effectiveness of entire drug classes—if such verification has not yet been conducted. Replication should be financed from public research funds to minimize conflicts of interest. Institutions previously seen as impartial authorities, including Cochrane and the WHO, must be subjected to rigorous scrutiny regarding their financial and institutional conflicts of interest.
3. FINAL REMARKS
What we currently have is not a health system, but a pharmaceutical-driven disease management system. To truly serve public well-being, its core foundations must be redefined. Health is a human right. Under optimal conditions, it should be a given—and must never be dictated by financial interests or political agendas. We need a new approach that has the wellbeing of all people in mind and is based on sound scientific evidence and the laws of nature. In particular, mental health and the ability to reflect and form opinions are the basis for free and democratic societies. The present proposal for a reform program is essentially aimed at enabling and stabilizing new systems. For decades, people have been conditioned to relinquish personal responsibility for their health to the medical system. This was done purposely to make people dependent on pharmaceutical drugs. The new system must re-empower individuals to restore their capacity for autonomous self-regulation. The principle of self-determined choice in one’s personal path to health must remain a fundamental human right—rooted in informed consent.
Under no circumstances does the system have the authority to impose mandatory medical interventions under the pretense of serving the “greater good” when, in reality, such measures advance pharmaceutical and political agendas.
We trust that this document will serve as a stimulus for discussion around the world, and invite you to discuss, expand and refine the concept encapsulated in this outlined of a health system reform program with focus on prevention and causal therapy.
Acknowledgements
This document was authored by Michael Nehls, MD, PhD. Christof Plothe, DO, contributed by preparing it for international publication and offering select additions.
Michael Nehls is a German physician and molecular geneticist. As a researcher, he deciphered the genetic causes of various hereditary diseases at German and international research institutions, publishing three of his discoveries in collaboration with several Nobel laureates. His discovery of a key gene in the development of immunity was honored as a "Pillar of Immunology" by the prestigious American Association of Immunologist. A science writer with a talent for making complex issues accessible to a wide audience, he has written several best-selling books that have been translated into many languages. As a private lecturer, he is a popular speaker at conferences and universities. You can learn more about Michael Nehls at www.michael-nehls.com. The original German version of this document can be found here.
Christof Plothe is a German osteopath, speaker and author, working in the field of integrative medicine, combining naturopathy, environmental medicine, and holistic dentistry with conventional medicine. He is on the board of EbMCsquared Community Interest Company (CIC), the Steering Committee of the World Council for Health (WCH), and also fulfils the role of WCH Health & Science Team leader. You can learn more about Christof Plothe here:
Web: www.christofplothedo.com and at www.worldcouncilforhealth.org:
X: https://x.com/ChristofPlothe
Substack: https://millivitalacademy.substack.com
“World Council for Health is grateful to collaborate with individuals and organizations from around the world, and endeavors to share such expertise in the pursuit of health and sovereignty for all people.”